Have you ever heard someone say, “My diabetes got worse and now I need insulin - does that mean my type 2 turned into type 1?” It’s a very common question, and it’s easy to see why people wonder about it. Both conditions involve problems with insulin and blood sugar, and both can lead to needing insulin treatment. But the truth might surprise you.
In this blog, we’ll talk in very simple words about an important question:
Can type 2 diabetes turn into type 1?
We’ll explain:
- What type 1 and type 2 diabetes really are
- Why one doesn’t become the other
- How symptoms can overlap and cause confusion
- How different lifestyles and herbal support can help
- What to do if your diabetes seems to be changing
By the end, you’ll have a clear understanding and feel confident about managing your health.
Understanding Diabetes: Two Very Different Conditions
Let’s start by looking at what each type of diabetes really means - in simple language.
What Is Type 1 Diabetes?
Type 1 diabetes is a condition where your body’s immune system mistakenly attacks the cells in the pancreas that make insulin. Without insulin, sugar cannot get from your blood into your cells for energy. That makes blood sugar rise.
This usually starts in childhood or early adulthood, but it can happen at any age. People with type 1 always need insulin because their body cannot make enough on its own.
What Is Type 2 Diabetes?
Type 2 diabetes is very different. In type 2:
- The body still makes insulin
- But the cells don’t respond to it well (this is called insulin resistance)
- Over time, the pancreas may make less insulin, but it doesn’t stop completely like in type 1
Type 2 usually develops in adults, but it can happen at any age, especially with risk factors like family history, lifestyle, and weight.
So, Can Type 2 Diabetes Turn into Type 1?
No - type 2 diabetes does not turn into type 1 diabetes.
They are completely different conditions with different causes:
- Type 1 is an autoimmune condition - the body destroys insulin‑making cells.
- Type 2 is a metabolic condition - the body can’t use insulin well.
You might hear people say that their condition “got worse,” or they now need insulin, but that doesn’t mean type 2 turned into type 1. It simply means their type 2 diabetes became harder to manage over time.
Why People Think One Type Can Turn Into the Other
Here are some reasons this misunderstanding happens:
1. Insulin Is Used in Both
Many people with type 2 end up using insulin as their condition progresses. This can make it feel like type 2 has changed into type 1 - but insulin use does not change your diagnosis.
2. Symptoms Can Look Similar
Both types can cause:
These overlapping signs can be confusing.
3. Late‑Onset Type 1 Can Be Misdiagnosed
Some adults develop a slow form of type 1 diabetes called LADA (latent autoimmune diabetes in adults). Because it starts slowly, it’s sometimes first mistaken for type 2 - but it is actually type 1.
How Do Doctors Tell the Difference?
Doctors use specific tests to understand which type of diabetes a person has, such as:
- Blood sugar tests (like fasting glucose or HbA1c)
- C‑peptide tests (to see how much insulin the body is making)
- Autoantibody tests (to check for autoimmune activity)
These tests help clarify whether someone truly has type 1, type 2, or a mix of characteristics, even if the symptoms look similar.
Why Does Type 2 Sometimes Get “Harder to Control”?
As type 2 diabetes progresses, many people find their blood sugar is more difficult to keep in range. This may be due to:
- Decreased insulin production over time
- Increased insulin resistance
- Unhealthy eating patterns
- Sedentary lifestyle
- Stress and sleep problems
When blood sugar becomes harder to manage, doctors might add medications or begin insulin - but this is still type 2, not a transformation to type 1.
Natural Support for Managing Type 2 Diabetes
While medications can be necessary, many people find that lifestyle and natural approaches help support blood sugar balance and overall well‑being. These suggestions don’t replace medical advice, but they can support you every day.
1. Eat Whole, Plant‑Based Meals
Focus on meals that are balanced and vegetarian, such as:
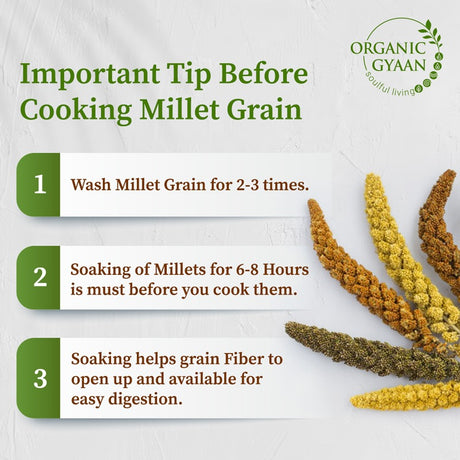
- Millets (like foxtail, little, barnyard) - slow to raise blood sugar
- Pulses and lentils - great protein and fiber
- Leafy greens and vegetables - packed with nutrients
- Healthy seeds (flax, chia, sunflower) - good fats and fiber
These foods help your body use glucose more steadily.
2. Use Traditional Herbal Powders
Many cultures use herbs to support metabolic balance:
- Fenugreek (methi) - supports glucose metabolism
- Cinnamon - may help with insulin sensitivity
- Amla powder - rich in vitamin C
- Turmeric - anti‑inflammatory support
These are supportive, but should be used as part of a balanced diet.
3. Stay Hydrated
Water is simple but powerful. Drinking water regularly helps:
- Prevent dehydration
- Support digestion
- Help the kidneys flush out excess sugar
Avoid sugary drinks, which can raise blood sugar quickly.
4. Be Active Every Day
Movement helps your cells respond to insulin more effectively. It doesn’t have to be intense:
- Walking
- Gentle yoga
- Stretching
- Household activity
These boost energy and help balance blood sugar.
5. Reduce Stress and Sleep Well
Chronic stress and poor sleep make blood sugar harder to control. Try:
- Deep breathing
- Meditation
- Regular sleep schedules
These support both your mind and body.
What About Gestational Diabetes and Prediabetes?
It’s important to know that:
- Gestational diabetes (during pregnancy) does not become type 1 or type 2 automatically - but it increases the chance of type 2 later.
- Prediabetes is an early stage where blood sugar is elevated but not high enough for diabetes - and it can be reversed with lifestyle changes.
But again, type 2 does not convert into type 1.
When to Talk to a Doctor
You should see a healthcare provider if:
- You notice symptoms like constant thirst, sudden weight changes, or extreme tiredness
- Your blood sugar numbers are rising or hard to control
- You feel confused or your symptoms change abruptly
A doctor can test and clarify your diagnosis and offer a plan that suits your needs.
Conclusion
So, the answer to the question can type 2 diabetes turn into type 1 is clearly no. They are separate conditions with different causes - even though they share some common symptoms.
Misunderstandings happen, especially when insulin becomes part of the treatment for type 2. But needing insulin doesn’t mean your condition changed - it means your body needs extra support.
What does matter is how you take care of your body every day. Choosing wholesome vegetarian foods, staying active, managing stress, and drinking enough water can make a real difference in how you feel.